Male Fertility Optimization
At Home Sperm Testing with Expert Physician Analysis and Treatment
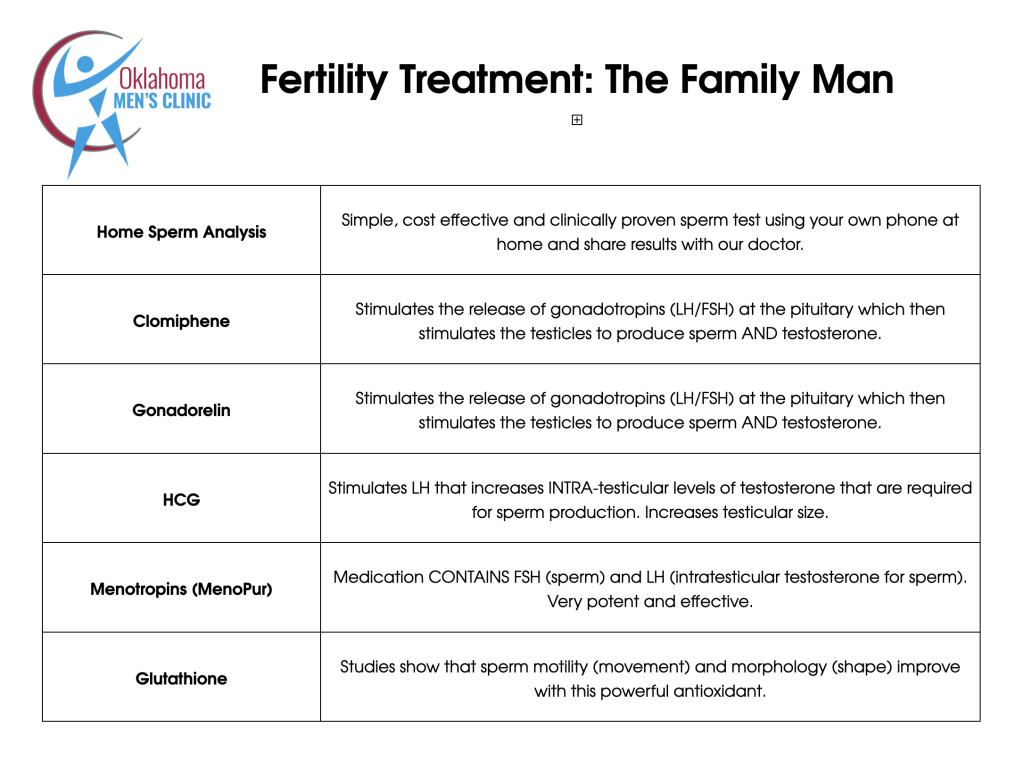
At Oklahoma Men’s Clinic, we utilize a convenient at home sperm analysis product for fertility that you can purchase HERE. The process is very simple to have your sperm analyzed at home with the results conveniently being sent to our expert physicians who will analyze your results and provide you with a comprehensive fertility treatment plan.
Male factors contribute to roughly 40% of infertility cases. Even when a male problem hasn’t been formally diagnosed, improving sperm health often makes the difference between failed and successful conception — whether naturally, with IUI, or as part of IVF. Fertility is a team effort: optimizing male reproductive health strengthens the foundation for conception and healthy pregnancy outcomes.
Sperm are highly responsive to their environment. Because they are sensitive, targeted lifestyle, nutritional, and medical interventions can produce measurable improvements in count, motility, morphology, and DNA integrity. Meaningful change usually requires consistent action over several months (spermatogenesis takes ~70–90 days).

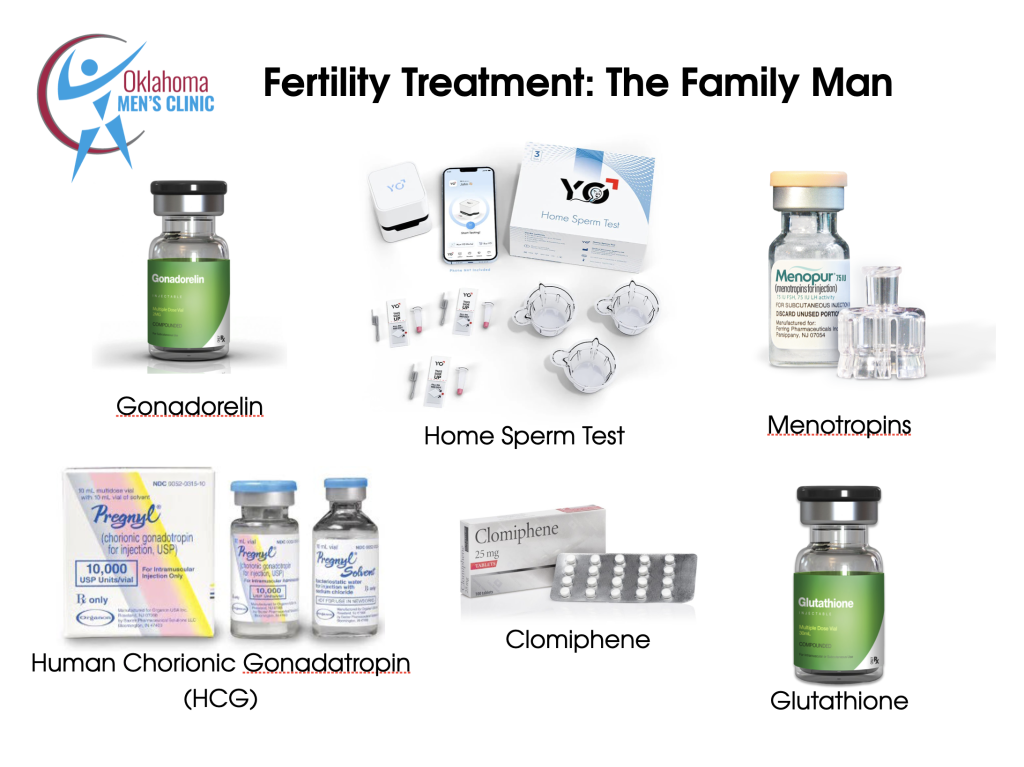
Treatment Options
Family Man Plan with Testosterone Therapy, 24 or 48 week programs
Family Man Plan without Testosterone Therapy, 24 week program
Comprehensive Fertility Approach
Key Nutrient Add Ons
Glutathione Injections are one of the more evidence-backed adjuncts for male fertility support.
How Glutathione Support Male Fertility
Master Antioxidant
Glutathione (GSH) is the body’s most powerful intracellular antioxidant.
Sperm are highly vulnerable to oxidative stress, which damages membranes, impairs motility, and fragments DNA.
GSH protects sperm cell membranes and DNA from reactive oxygen species (ROS).
Improved Sperm Parameters
Clinical studies have shown that glutathione therapy can improve sperm motility, morphology, and vitality, particularly in men with oxidative stress-related infertility.
It helps stabilize the midpiece of sperm (where mitochondria are located), improving energy production and motility.
Detoxification Support
Glutathione supports liver detox pathways and helps clear heavy metals and environmental toxins — both of which can impair spermatogenesis.
Evidence from Studies
Randomized trial (1992, Lenzi et al.): 600 mg glutathione injections every other day for 2 months improved sperm motility and morphology in infertile men with varicocele and other conditions.
Other small trials: Show improvements in motility and morphology, especially in men with idiopathic infertility or oxidative stress markers.
Injectable vs Oral/IV
Injectable glutathione: Higher bioavailability, more direct impact on oxidative stress.
Oral glutathione: Limited absorption, though liposomal forms are somewhat better.
Intramuscular (IM) injections: Commonly used in fertility protocols when labs show oxidative stress or high sperm DNA fragmentation.
Glutathione injections may significantly improve sperm quality in men with oxidative-stress-related infertility. They’re best used as part of a comprehensive male fertility optimization protocol that includes nutrition, lifestyle, and targeted micronutrient support.

Comprehensive Options for the Oklahoma Man
1) Foundations — Nutrition & Supplementation
What you eat and absorb directly affects sperm production and quality.
Diet approach
Emphasize whole, nutrient-dense foods: wild-caught fish, pastured meats, high-quality fats, colorful vegetables and fruits, nuts and seeds.
Prefer organic produce when possible to minimize pesticide exposure.
Key nutrients & supplements
Antioxidants (e.g.,vitamin C, vitamin E, coenzyme Q10): protect sperm DNA and improve motility.
Minerals: zinc (testosterone, ejaculate volume), iodine and selenium (thyroid & reproductive health).
Amino acids: L-carnitine, D-aspartic acid — support sperm energy and structure.
Targeted botanicals/adaptogens: selected agents such as Shilajit are commonly used to support testosterone and vitality.
Injectable antioxidants (e.g., glutathione) can be considered when testing shows high oxidative stress or DNA fragmentation.
Supplements should be evidence-based, high-quality, and tailored to labs and history.
2) Food As Medicine — High-Impact Choices
Small dietary swaps can be powerful:
Oysters — concentrated zinc and D-aspartic acid.
Pomegranate — antioxidant support for motility and morphology.
Tomato products (lycopene) — associated with improved sperm structure/DNA stability.
Pumpkin seeds / pumpkin seed oil — zinc, essential fats, prostate support.
These foods complement targeted supplementation and broader dietary improvements.
3) Hormonal & Environmental Balance
Optimizing hormones and reducing harmful exposures are central:
Comprehensive hormonal assessment: testosterone, estradiol, LH/FSH, DHEA, prolactin.
Metabolic & micronutrient screens: iron studies, thyroid function, vitamin D, etc. Both low and high iron can impair fertility.
Lifestyle & environmental risks:
Avoid prolonged scrotal heat (tight underwear, frequent saunas/hot tubs).
Reduce exposure to endocrine-disrupting chemicals and heavy metals.
Address chronic stress and poor sleep — both affect hormone balance and sperm quality.
Detox support: when indicated, gentle liver-support botanicals and mineral therapies may be used as adjuncts; these should be individualized.
All advanced interventions require informed consent and frequent laboratory follow-up.
The Bigger Picture
Male fertility reflects whole-body health. Improvements in sperm parameters often coincide with gains in energy, mood, sleep, and libido. This protocol is a flexible, evidence-informed framework: individualized plans based on labs, exposure history, and reproductive goals produce the best outcomes. With consistent implementation and clinical oversight, non-invasive approaches frequently yield significant improvements — often reducing the need for more invasive fertility treatments.


